Better Data Collection Essential to Understanding and Addressing Health Inequities
December 14th, 2022
The COVID-19 pandemic exposed and exacerbated the weaknesses of the U.S. health care system and highlighted long-standing inequities for minority communities. Highlighted during this period was the profound impact of economic stability, education, social and community life, one’s neighborhood and access to high-quality health care—social determinants of health—on the overall health and well-being of communities.
As a result, addressing health inequities has become a top priority for many employers, purchasers and health care providers. The ability to effectively collect a range of data points about patients and the care they receive is an essential component to creating meaningful change and ensuring populations achieve their full health potential.
Looking at health quality data by race, ethnicity, language and other patient characteristics, is crucial for understanding how long-standing systems of privilege and oppression impact the health of minority populations and communities. However, patient self-reported race, ethnicity and language (REaL) data across health insurance markets is widely variable and overall limited. While race and ethnicity data in California’s Medicaid program (called Medi-Cal) is broadly available likely because of legislation requiring health plans to collect this information starting in 2009, corresponding data for the majority of patients who receive health benefits through the commercial market – via employers or on the private market –is low or absent.
These limitations of known race and ethnicity data hinder the ability to see where disparities exist and for the health system to react with meaningful interventions. For health plans and large employers and purchasers, who provide health benefits for more than half the U.S., it is crucial to uncover variation in the access to care and the quality and experience of care being provided.
With better self-reported patient demographic information, employers, purchasers, payers and providers can tie this data to health care access, quality, patient experience and outcomes to illuminate exactly where disparities exist. These insights can enable tailored interventions and support for improvement.
How to Improve Data Collection
Legislation, Policy and Regulation
Legislation and regulations can incentivize or require health plans, providers and other health system organizations to increase the collection and quality of self-reported demographic data. Legislation and statute also have the potential to enforce standardization for data fields and definitions, which enables largescale purchasers of health care to align with their health plan and provider industry partners and enhance their ability to share, aggregate or disaggregate data to identify trends and implement plans for improvement.
It is crucial to ensure that national and state standards do not contradict each other.
Contracting and Business Relationships
Contracting requirements and incentives as part of large-scale public and private purchaser and payer programs can increase the collection, reporting and use of REaL data and thereby bolster efforts to mitigate disparities. Large purchasers could add incentive payouts if plans are able to stratify measures across self-reported REaL data. Health plans, provider organizations and other payers that contract within the health system can use incentive payouts for better data collection and stratification and other efforts to reduce disparities. Another approach is to build tiered networks that point patients to providers who have proven to be stronger at collecting, reporting and using REaL data.
It is important for purchasers and payers to avoid siloed initiatives that conflict with each other.
Organizational Leadership, Systems Structure and Culture
Organizations that pay for services at the point of care (e.g., health plans and independent physician associations, or IPAs) have the potential to increase REaL data collection, reporting and use by assessing and enhancing data collection opportunities, sharing data internally and creating a culture that values the collection of this information. This starts with organizational leadership. It is important to normalize data collection into regular workflows to improve the quality and ensure the most accurate information possible.
Purchasers, health plans and provider organizations can increase patient self-reporting by increasing awareness of how the data will be used and educating enrollment counselors and other staff with direct patient interaction on why it is important to collect this data.
Certification Requirements
The National Committee for Quality Assurance (NCQA) has required plans to report their percentage of self-reported REaL data for certain key measures, with a goal of 80% self-reported data. Additional accrediting organizations, purchasers and others could adopt similar certification requirements to support reporting and stratification for the same measures and self-reported data goals as NCQA. This would increase the consequences for not aligning and support the overall goal of greater availability of self-reported REaL data.
Read more in our latest issue brief.
Opportunities in COVID-19 Vaccine Access and Equity
May 4th, 2021
While COVID-19 vaccine eligibility has expanded and supply has increased, data show that access to vaccines are not equitable throughout California’s communities.
Health care leaders are looking to work together differently as their vaccination efforts shift from trying to meet demand through mass vaccination sites to targeted interventions that address the needs and concerns of high-risk communities and vaccine-hesitant individuals.
In late April, PBGH’s California Quality Collaborative (CQC) hosted a closed roundtable discussion for health plans, provider groups and California state agency representatives to discuss challenges and success stories in their efforts to distribute COVID-19 vaccines and support equitable vaccine distribution for under-resourced populations. Five key actions stakeholders need to take emerged from the conversation:
1. Invest internally in policies supporting equity. During the past year, many organizations worked to improve internal processes that would better enable them to serve the diverse needs of their members and staff. L.A. Care Health Plan, the nation’s largest public health plan with nearly 2.2 million members, for example, developed a set of more robust internal policies to address diversity and inclusion, as well as programs designed to minimize barriers in working with minority or women-owned businesses, an approach described in the Clinical Improvement Network Connections spring 2021 publication.
2. Facilitate real-time data sharing. All groups agreed that, while there had been investments in data-sharing that facilitated collaboration to distribute and ensure access to vaccines, there were still gaps between health care delivery systems, public health and community-based organizations in terms of the accuracy of, and timeliness with which, essential clinical data was shared. As we begin to recover from the pandemic work should be done to ensure real-time data-sharing, especially between the California Immunization Registry and health information exchanges and organizations not traditionally part of health care information exchanges.
3. Provide clear, consistent and trusted communication. It was extremely important for all entities to streamline, test and regularly deliver communications campaigns to stakeholders, including community members, provider groups and member patients.
4. Leverage trusted relationships from primary care providers. Primary care providers were unable to play a significant role in the early days of vaccine distribution, often because mass vaccination sites were prioritized so individual practices received limited vaccine supply or were unprepared to accommodate the stringent storage requirements. With vaccine distribution having stabilized, there is an opportunity to tap into the primary care provider community, which is positioned to leverage long-standing patient relationships and play an important role in vaccination efforts. Increasing primary care’s role in COVID-19 vaccine administration may prove extremely effective in reaching vaccine-hesitant or skeptical patients.
5. Sustain new and strengthened partnerships. Overall, there was a recognition that the public health emergency and response has illuminated how effective cross-sector collaboration between health plans, public health departments, provider groups and community-based organizations can be at solving urgent problems when working together. Now, there is a question about how partnering groups can continue to collaborate while finding ways to become more efficient.
COVID-19 Vaccine Resources
Patient Experience and Telehealth During COVID-19: Investigating Key Success Factors and Obstacles
February 26th, 2021
The global COVID-19 pandemic has led to a rapid increase in virtual care delivery that will likely be long-lasting. During the height of the pandemic, fear of infection and stay-at-home orders meant that many practices stopped seeing most patients in person for routine care. Relaxing of government regulations allowed for widespread national adoption of telehealth.
Telehealth holds great promise for improving primary care through increasing access, improving patient experience and enabling team-based care models. Importantly, while telehealth expands access to all patients, it may improve health equity for lower socio-economic patients who may lack transportation or sick leave.
To gather the patient perspective on telehealth, The Purchaser Business Group on Health developed and fielded a telehealth patient experience survey as part of the Patient Assessment Survey (PAS) program. Approximately 12,000 surveys were distributed by email to patients with commercial and Medicare coverage who had a virtual visit (phone or video) with a primary care provider in California; 1,500 email responses are reflected in the research findings.
Key Findings
- Equal satisfaction between virtual and in-person care: No significant differences were found in ratings of patient visits between telehealth and the regular PAS survey responses (which measure in-person care).
- Telehealth was popular: A total of 87% of survey respondents recommend telehealth; of survey respondents, 73% want to continue using telehealth in the future.
- Video visits were favored over audio-only: Ratings of visits and communications were nearly identical in video and telephonic visits, but patients who reported that they would likely recommend telehealth and engage in repeat telehealth visits significantly favored video appointments.
- Provider communication was good: Most patients said the provider with whom they met via telehealth methods explained information in a way that was easy to understand (92%), listened carefully (92%), spent enough time with them (91%) and had relevant patient medical history on hand during the visit (88%).
- Most patients received medical tests: Half of survey respondents had tests ordered by their provider. Most followed up to have the tests conducted (84%), and most patients were able to access their test results (88%). Patients were most likely to get the tests ordered on their behalf while being seen for COVID-19 concerns, whereas patients being seen for chronic health care or other health issues were least likely to have tests ordered for them. Patients who did not receive ordered tests (16%) scored their health care provider lower on communication scores.
Despite these promising findings, PBGH research has been, to date, limited to commercial populations in the state of California. Further research on patient experience and clinical outcomes should be conducted nationwide with more diverse populations, including Medicaid beneficiaries, racial and ethnic minorities and those with limited English proficiency. PBGH will have preliminary results from a survey with a sample of patients with Medi-Cal coverage in Spring 2021 and seeks to expand this measurement nationwide.
Implications
The findings of the PBGH Telehealth Survey are instructive for provider organizations, solution providers and health plans. The survey findings suggest the following four steps can make a meaningful difference in ensuring that patients have a positive experience with telehealth:
- Continue to offer telehealth. Patients enjoy telehealth and want to continue using virtual care in the future.
- Offer video visits. Satisfaction with telephonic and video care was high, but users of video visits were more likely to recommend telehealth and want to continue using telehealth.
- Provide instructions for video visits. Patient satisfaction is highest when clear instructions are provided to the patient in advance of a video visit.
- Offer both virtual and in-person care options. Patients indicated the need for in-person options to evaluate certain physical concerns, such as broken bones or rashes. Patients feel they can determine if an in-person appointment versus virtual care is appropriate for their unique health issues.
Read the full report.
Primary Care Practices Can Engage Patients in Virtual Care
June 6th, 2020
During the most challenging phases of the COVID-19 pandemic, one opportunity for the health care delivery system has been the rapid adoption of telehealth and virtual care by both primary care practices and patients. The Pacific Business Group on Health’s California Quality Collaborative (CQC) has hosted webinars to support and spread successful practices in virtual care for independent primary care practices and IPAs as they rapidly implemented telehealth technology and workflows.
Nationally, the trends reflect widespread virtual care adoption. By one May 2020 analysis, telehealth visits in the US increased 300-fold in March and April 2020 compared to the same time period in 2019 (Epic Health Research Network). Providers have been pleased with their telehealth experience, and patients have too: 88% of patients new to telehealth said they would like to use it again (PwC Health Research Institute). The health system is eager to build on the implementation gains around virtual care made during the public health emergency, especially its ability to improve access to care and reduce costs.
Patient engagement in virtual care
Yet today, more than ever, it’s essential for health care clinicians and care teams to ensure that virtual care being provided is as patient-centered as possible. This topic was the focus of a May 6 webinar hosted by CQC, which highlighted presentations from a number of experts including Dr. Courtney Lyles, Associate Professor, Center for Vulnerable Populations at UCSF; Libby Hoy, Founder & CEO, PFCC partners; and Dr. Fiona Wilson, former Teladoc provider and current Supervising Clinician Specialist, Workers Compensation Division, Department of Human Resources, City & County of San Francisco.
Dr. Lyles shared examples from decades-long research done around patient portals, telephone visits and tactics that help bridge the “digital divide,” even in regions of strong technology adoption, such as the Bay Area. Her advice was not to make any assumptions about what patients do or do not have access to, and establish ongoing trainings, where patients can be assured to get continuous support for the virtual care they are seeking.
Libby Hoy of PFCC partners shared lessons from her organization’s history building patient advisory capacity. She cautioned that the work, especially at this time, is messy, but reminded care teams and providers that involving patients in the design process of the workflows results in more effective care.
Dr. Wilson shared her experience as a telehealth provider during COVID-19 for Teladoc, an organization that provides virtual care for patients all over the United States. Her advice for clinicians was to be an empathetic and engaged listener to patients when they are sharing their health issues, and make sure to ask about non-medical needs that may be even more present today, such as social isolation and economic hardship.
What providers can do now
Today, primary care practices are regrouping after shelter-in-place restrictions lift, adapting to a hybrid of virtual and in-person care, and working to address any care needs of their patients that were deferred during the height of epidemic. Yet even in this time of transition, CQC’s expert panelists shared the following steps practices can take to focus on patient needs:
- Always ask patients their preferences. Ask what technology they have access to, and what makes them comfortable. Make sure your visit builds on your relationship, addresses what device they are using and that you ask how you can be of help during this process.
- Look to your patients and families as resources to designing your telehealth programs. Outside even the visit, consider implementing patient open-ended surveys, focus groups, telephone calls or advisory programs. Tap into the people with the least experience to help you improve your work.
- Make workflows as simple as you can. Technology can be part of the barrier, but at the same time, almost everyone has a phone. Start with the tools that you and patients have. You don’t need a smart phone to conduct these visits.
Access CQC’s May 29 webinar recording and summary here.
Doctors Expect to Use Telehealth More Extensively Post COVID-19
April 27th, 2020
Physicians Embracing Telehealth During Pandemic
Telehealth is quickly emerging as an important clinical tool for physicians scrambling to adapt to the COVID-19 pandemic. Both patients and physicians report being happy with treatment delivered via telehealth, but doctors say barriers to adoption still exist.
Two April surveys conducted by the Pacific Business Group on Health’s California Quality Collaborative, during a webinar with independent physician associations (IPAs), community health clinics and managed services organizations, found that more than 80% of polled physician practices in California are presently using telehealth to deliver care.
Most practices report having launched telehealth services in earnest only in the three-to-four weeks after the pandemic’s shelter-in-place orders rolled out. Providers are using a combination of both telephone and video technologies not only for COVID-19 patient screening, but also urgent care, wellness visits and other clinical services.
Nearly three-quarters of poll respondents said clinicians were satisfied or very satisfied with providing care via telehealth.
Nonetheless, uncertainties remain about payment, policy and patient uptake of this technology. About one-third of respondents said policies on payment for telehealth were confusing or very confusing, and 64% said they need more guidance from health plans on billing.
Notably, about 40% of IPA representatives said they were extremely or very worried about their organizations’ financial health, while another 47% said they were somewhat worried.
During CQC’s webinars, IPAs and small physician practices identified a range of additional barriers to launching or expanding telehealth, including:
- Helping patients adopt telehealth, notably older patients without smartphones or with low digital literacy
- Reaching hard-to-find patients, like homeless patients without phones
- Improving patient acceptance and technical training (providers did note that when patients tried telehealth, they generally liked it)
- Providing staff training
- Documenting and coding for telehealth visits
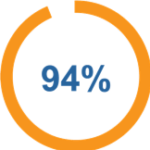
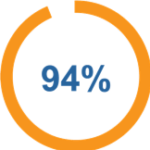
Despite the challenges, there’s broad agreement that the COVID-19 epidemic has helped to push past resistance to the more widespread use of telehealth; 94% of IPA respondents tell PBGH that they expect to use telehealth differently or more extensively once the pandemic begins to abate.